What is Lipedema?
Lipedema is generally described as a chronic and generally progressive fat tissue disorder that almost exclusively affects women. It is characterized by a symmetrical enlargement of the lower body due to excessive fatty deposits from waist to the ankles, and patients also suffer from easy bruising, orthostatic edema, and pain. The condition is often confused with simple obesity, but often the fat deposits aren't changed by weight loss. They can't be starved or exercised away.
Heredity seems to play a part, and the onset of symptoms seems to coincide with times of significant hormonal upheaval, such as during puberty, pregnancy and menopause (Szel et al, 2014). Besides the disproportion between upper and lower body that occurs with lipedema, the most devastating feature may be that it is generally believed to be non-responsive to diet and exercise. First reported by physicians at the Mayo Clinic in 1940 (Wold, Hines & Allen, 1951), this condition continues to remain a poorly understood, largely under diagnosed, and profoundly impactful syndrome.

The Lipedema Project 2015-2019. All rights reserved. Used with permission.
-------------------------------------------------------------------------------------------------------
SPECIAL ANNOUNCEMENT: Support Lipedema Research!
Consider donating to The Lipedema Project, a 501c3 non-profit organization, by participating in this fundraiser here. All funds will be specially earmarked for lipedema research.
--------------------------------------------------------------------------------------------------------------
Gender and Lipedema
Gender is a major determinant of adipose tissue distribution. Research has shown that in general men are more prone to lipolysis, or fat burning, and women tend more toward lipogenesis, or fat creation and storage (Varlamov et al., 2015). Additionally, women have a tendency toward upper body lipolysis and lower body lipogenesis which may result in a lipedema presentation.
During puberty, females increasingly store subcutaneous fat throughout the body, with concentrations at the hips, buttocks and thighs. Women tend also to be more sensitive to insulin, the fat storage hormone, which puts them at higher risk for weight gain than men (Cignarella & Bolego, 2010).
Although considered by some clinicians to not be a lymphatic disorder, lipedema is a condition of concern because disrupted lymphatics are often a constituent of the condition. For instance, most women with this condition have some mild swelling and the increased sized of fat cells can interfere with lymphatic drainage. Hence, a significant number of patients tend to also develop lymphedema.
For more information visit the lipedema simplified website.
Keto for Lipedema
Dr Gabriele Faerber from Germany published an interesting paper in February 2018 in the journal Phlebologie. The title of the paper is “Obesity and Chronic Inflammation in Phlebological and Lymphatic Diseases.” Dr. Faerber reviews the literature related to this topic, suggesting a relationship between obesity, chronic inflammation and lymphatic disorders, then she shares some case studies from her own practice in Hamburg.
Dr Faerber comes to the conclusion that many of the complaints associated with lipedema such as pain, swelling, inflammation, and bloating, as well as the development of lymphedema and vascular malfunction in later stages of lipedema, increase in severity when abdominal obesity is also present. She discusses how inflammation and hormonal factors play a much stronger role in women with lipedema who also have increased abdominal fat.
She then makes the case for using a ketogenic diet to mitigate all of these factors. Dr. Faerber argues that keeping to low glycemic foods, avoiding snacking and eating less frequently, and eliminating sugar-free sweeteners has been very successful eating plan for her patients with lipedema. Weight loss, even from the lower body, seems to be achievable for the first time. More than 80% of her patients with lipedema have reduced or resolved pain and edema. Because these results are also seen in women with lipedema who are normal weight, she believes that these fantastic results are not only from weight loss, but are because of the reduction in swelling and inflammation that is achieved with a ketogenic diet.
Over 13,000 women with lipedema have joined the Keto Lifestyle for Lipedema Facebook group for support, recipe/meal planning ideas and resources. The latest research is commented upon and lively supportive conversation is supported. This is a closed group and is only available to women.
References
- Szel, E, Kemeny, L, et al. (2014). Pathophysiological dilemmas of lipedema. Medical Hypotheses, 83, 599-606.
- Wold, LE, Hines, EA & Allen, EV. (1951). Lipedema of the legs: A syndrome characterized by fat legs and edema. Annals of Internal Medicine, 34(5), 1243-1250.
- Varlamov, O, Bethea, CL & Roberts, CT. (2015). Sex-specific differences in lipid and glucose metabolism. Frontiers in Endocrinology. 5(241). doi:10.3389/fendo.2014.00241.
- Cignarella, A & Bolego C. (2010). Mechanisms of estrogen protection in diabetes and metabolic disease. Hormone Molecular Biology and Clinical Investigation, 4(2), 575-580. doi: 10.1515/HMBCI.2010.084.
Other Suggested Reading
Lipedema - The Disease They Call FAT by Erez Dayan, Julie N. Kim, Mark L. Smith, Catherine A. Seo et al.
All About Lipedema by Dominik Dr. von Lukowicz and others
(Please Note: As an Amazon Associate, I earn from qualifying purchases.)
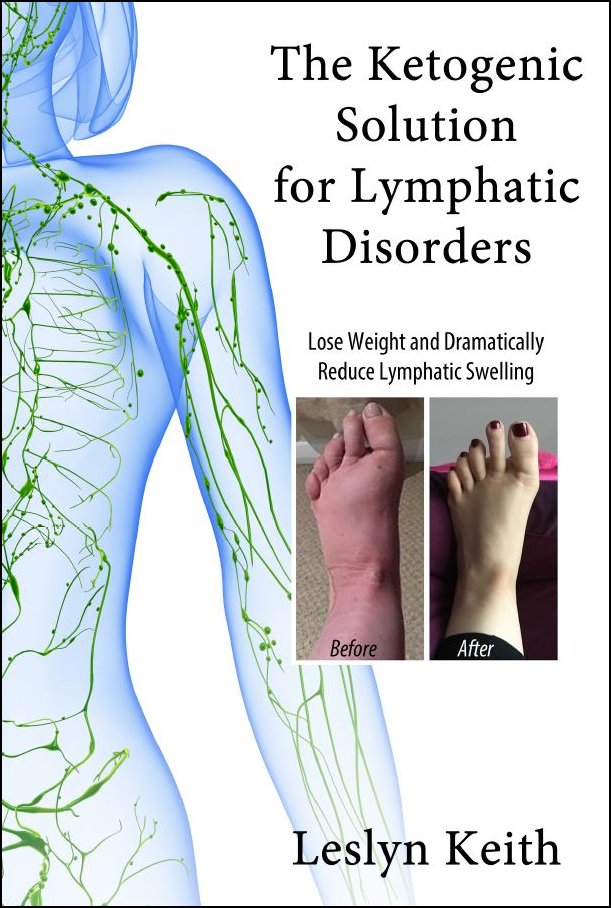
Books by Leslyn Keith, OT
|
Buy the print softcover book on Amazon Buy the E-book via Paypal |
Buy the print softcover book on Amazon Buy the E-book via Paypal |
Follow Leslyn Keith on YouTube!
Done with Lipedema, back to Home